2D Echo (Echocardiography)
2D Echocardiography, also known as 2D Echo, is an ultrasound test that uses sound waves to create real-time, two-dimensional images of the heart. Doctors use it to assess the structure and function of the heart. By visualizing the heart in motion, a 2D Echo provides critical information about the heart’s chambers, valves, and blood flow.
How 2D Echocardiography Works
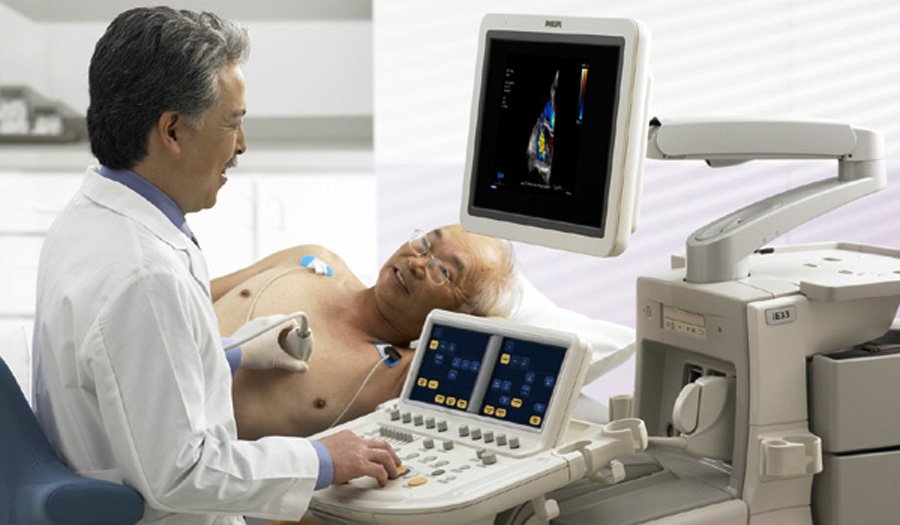
During a 2D Echo, a technician places a small device called a transducer on the chest and transmits high-frequency sound waves into the body. These sound waves bounce off the heart’s structures and convert them into images displayed on a monitor. This procedure allows doctors to observe the heart’s size, shape, and movement in real time.
Components of the 2D Echo Test
- Transducer: The handheld device that emits sound waves and receives the echoes from the heart.
- Gel: The technician applies a conductive gel to the chest to ensure clear transmission of sound waves.
- Monitor: The technician displays the images produced by the ultrasound on a monitor for the healthcare provider to analyze.
Key Information Provided by a 2D Echo
- Heart Chambers: A 2D Echo helps doctors visualize the four chambers of the heart: the left and right atria and the left and right ventricles. It shows their size, thickness, and any abnormalities such as enlargement or thickening.
- Heart Valves: The test provides information about the heart’s four valves (mitral, aortic, tricuspid, and pulmonary). Doctors use it to detect valve dysfunctions such as stenosis (narrowing) or regurgitation (leakage).
- Wall Motion: Doctors assess the ability of the heart’s walls to contract and pump blood. This is particularly important for detecting damage from a heart attack or ischemic heart disease.
- Blood Flow: The test allows doctors to evaluate blood flow through the heart and major blood vessels. Doctors can detect abnormalities in blood flow, such as regurgitation (backflow) or shunting (abnormal flow).
- Pericardium: The technician evaluates the outer layer of the heart, called the pericardium, for any signs of thickening or fluid buildup (pericardial effusion).
- Ejection Fraction: This measures the percentage of blood pumped out of the heart with each contraction. A low ejection fraction can indicate heart failure.
Indications for 2D Echocardiography
Doctors often recommend a 2D Echo when a patient presents with symptoms or risk factors that suggest a heart condition. Common indications include:
- Chest pain or discomfort
- Shortness of breath
- Fatigue or weakness
- Palpitations (irregular heartbeats)
- Swelling in the legs or ankles (a sign of heart failure)
- Dizziness or fainting
- Heart murmur (abnormal heart sound detected by a doctor)
- Known heart disease or to monitor ongoing heart conditions
Types of 2D Echocardiography
Doctors use several variations of 2D echocardiography depending on the clinical need:
- Transthoracic Echocardiography (TTE): The most common type, performed by placing the transducer on the chest. It is non-invasive and does not require sedation. Doctors often use TTE for general heart evaluations.
- Transesophageal Echocardiography (TEE): This type involves passing a flexible tube with an ultrasound probe down the patient’s throat to capture clearer images of the heart. Doctors use TEE when images from a transthoracic echo are unclear or when more detailed information is needed.
- Doppler Echocardiography: This variant uses Doppler ultrasound to evaluate blood flow. It helps doctors assess the speed and direction of blood flow through the heart and blood vessels, providing additional details about valve function and cardiac output.
- Stress Echocardiography: This test involves performing an echocardiogram before and after physical exercise or medication-induced stress. It helps doctors assess how the heart performs under stress, useful for diagnosing coronary artery disease or ischemic heart conditions.
Benefits of 2D Echocardiography
2D Echo offers the following benefits:
- Non-invasive: It is a painless procedure that does not require surgery or injections.
- Real-time imaging: It provides immediate images of the heart in motion, allowing for rapid diagnosis and decision-making.
- Safe: Unlike X-rays or CT scans, echocardiography does not involve radiation, making it a safer option for regular monitoring.
- Accessible: The 2D Echo is widely available in hospitals and clinics and is relatively affordable compared to other heart imaging tests.
- No preparation needed: Patients do not need significant preparations, although doctors may ask them to avoid heavy meals before the procedure.
Common Heart Conditions Diagnosed Using 2D Echocardiography
Doctors use 2D Echo to diagnose the following conditions:
- Heart Valve Diseases: Conditions like mitral valve prolapse, aortic stenosis, or regurgitation can be detected and monitored with 2D echocardiography.
- Congenital Heart Defects: Structural heart problems present at birth, such as holes in the heart (e.g., atrial septal defects or ventricular septal defects), can be diagnosed.
- Heart Failure: A 2D Echo helps doctors evaluate the heart’s pumping efficiency and diagnose heart failure based on abnormal ejection fractions or impaired wall motion.
- Cardiomyopathies: Conditions that affect the heart muscle, such as hypertrophic or dilated cardiomyopathy, can be visualized and monitored.
- Pericardial Effusion: Fluid accumulation around the heart (pericardium) can be seen, helping diagnose conditions like pericarditis.
- Endocarditis: Infection of the heart valves can be detected through valve abnormalities or the presence of vegetation (growths) on the valves.
Limitations of 2D Echocardiography
2D Echo has some limitations:
- Obesity or lung disease: Patients with excessive body fat or lung disease may have poor image quality because the sound waves have difficulty transmitting through thick tissue.
- Limited view of certain structures: Some parts of the heart, such as the posterior wall or parts of the left atrium, may be difficult to visualize with a transthoracic echo, which may require a transesophageal approach.
- Operator-dependent: The quality of the images can depend on the experience and skill of the technician performing the test.
